
Cannabis and Occupational Therapy
By Tauni Malmgren, OT/S and Emmy Vadnais, OTR/L
Backround
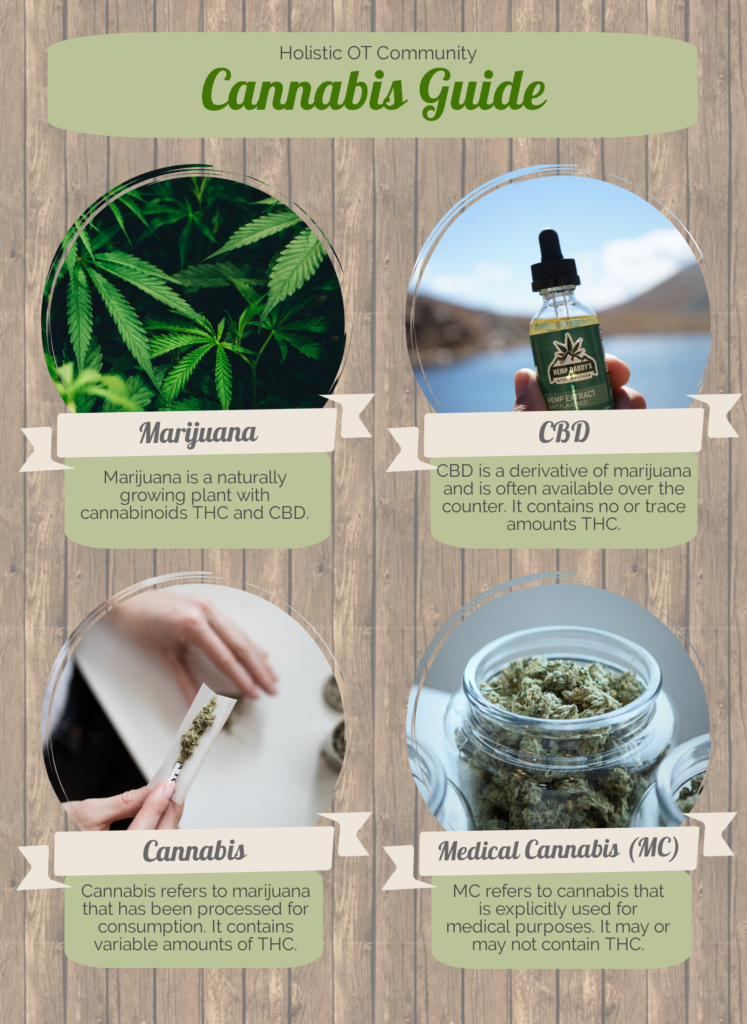
People have used cannabis for medical purposes for at least 3,000 years according to the National Center for Complementary and Integrative Health.1 Currently, medical cannabis (MC) is becoming legalized in many parts of the United States. MC simply refers to cannabis that is used medically. Cannabidiol (CBD) has also gained attention for its medical benefits. As this article will explain, all cannabis has CBD in it, but CBD is not cannabis. Recently, an article from the American Occupational Therapy Association (AOTA) addressed the importance of understanding MC to provide client education and support medication management to increase occupational performance.2
How Cannabis Works
Cannabis contains hundreds of chemicals called cannabinoids. The most well-known cannabinoids are Δ9-tetrahydrocannabinol (THC) and CBD. While THC has psychoactive agents that lead to intoxication, CBD does not have these agents. A report from the World Health Organization states that CBD has no addictive properties and is not a public health risk. CBD is an option for people wanting the benefits of MC without the psychoactive effects or risk for addiction.3
The Legality of Cannabis and CBD
In some states, cannabis is now legal and does not require a prescription, making it more accessible to the public. MC is also legal in some states after some researched benefits. As time goes on, with more people turning to MC, how it may benefit people as well as the risks and benefits may become more apparent. Here is a helpful map showing the legality of cannabis by state.
CBD oil has become more readily available in the states where it is legal and that does not require a prescription. For more up to date details on the legality of CBD oil, see this helpful map. Even though CBD exists in a legal gray area, CBD oil is ubiquitously sold as a supplement, and the FDA does not regulate the safety or purity of these medication. There are no set guidelines to know if a CBD product is labeled with accurate active ingredients or dosages. What’s more, it is unknown to the medical community currently what the most effective therapeutic dosage of CBD for a particular medical condition. There may be more clear guidelines and research about the possible benefits for CBD oil in the future. Until then, occupational therapy practitioners can pay close attention to companies and distributors of CBD and look out for indicators of better quality such as third party testing and more research.
CBD Benefits
In 2018, the U.S. Food and Drug Administration (FDA) approved a pharmaceutical grade CBD medication, Epidolex, for the treatment for two severe and drug-resistant pediatric seizure disorders, Lennox-Gastaut syndrome and Dravet syndrome. However, according to CBD Project, much of what our clients have access to are off market CBD oils that are widely accessible and largely unregulated.4 The project suggests that health professionals learn more about MC and CBD to adequately provide client education about dosages, modes of administration, cannabinoid synergies, risk factors, and drug interactions.
Some members of the Holistic OT Community have observed benefits for their clients who have used CBD in clinical practice where the CBD was prescribed by a primary practitioner or taken autonomously by the clients themselves. They have reported that CBD alleviated many symptoms and conditions including chronic pain, anxiety, post-traumatic stress disorder (PTSD), attention deficit hyperactivity disorder (ADHD), autism, and overall brain function. They also observed that CBD has helped with epilepsy, cerebral palsy, viral infections, seizures, muscle spasms, soft tissue repair, and cancer, and more generally improved sleep, digestion, skincare, and generalized inflammation.5
What Does the Research Say?
AOTA states that federal restrictions place major restrictions on the study of MC resulting in a lack of high quality clinical trials.2 Study limitations include small sample sizes, inconsistent outcome measures, and variable doses, types of cannabinoids, and methods for drug administration. While clinical trials are lacking, literature reviews have found evidence showing that MC can help adults with chronic pain, symptoms from chemotherapy, and muscle spasticity from multiple sclerosis (MS). Moreover, reports show that MC can help with epilepsy, PTSD, and side effects from HIV/AIDS.
Project CBD has a breakdown of the positive benefits of CBD and THC that are supported by scientific evidence.4 A study found that CBD and THC are neuroprotective agents with antioxidative properties that block neurotoxins, or poisons that act on the nervous system.6 Another study found that THC and CBD can facilitate the growth of new brain cells in adult mammals.7
A study explains the endocannabinoid system as regulatory system in the body impacting health and disease through the peripheral and central nervous systems and peripheral organs. This study states that modulating the activity of the endocannabinoid system through MC can positively impact a wide range of disparate diseases and pathological conditions including mental health disorders, biomechanical disorders, and much more.8 Another study explores more deeply the effects of MC on the endocannabinoid system.9
Methods of Cannabis and CBD Administration
Research says that MC can be inhaled (e.g., smoking cigarettes, pipes, water pipes, and vaporizing), taken orally (e.g., edibles, juice, tea, oils, capsules, tinctures, and lozenges), oromucosally (e.g., spray), and topically (e.g., creams and suppositories).10 The effects of inhalation have a maximum effect for 15-30 minutes and last for 2-3 hours. The oral route has a maximum effect for 1-3 hours and last for 6-8 hours. The oromucosal route has a maximum effect in 15-45 minutes and lasts for 6-8 hours. The topical route has variable, localized effects.

Potential Side Effects of Cannabis and CBD
An AOTA article states that “like many medication, cannabis has documented adverse effects.”2 These include impaired cognition, perception, and motor skills, increased risk for myocardial infarction, and increased risk of motor vehicle accidents. Long term adverse effects include impaired verbal learning memory, impaired attention, and if smoked, poor respiratory function. Moreover, heavy users are likely to report suicidal thoughts and regular users have increased risk of social anxiety disorders. However, the article notes that this sample was of people who used cannabis heavily for recreation. People who use MC report fewer adverse effects. However, according to the National Center for Complementary and Integrative Health, it is unknown whether the benefits outweigh the risks.11
When evaluating clients, the article states that acute MC may impair balance, so practitioners should monitor clients for fall risks and provide fall prevention strategies if necessary. Practitioners should also evaluate and monitor effects on cognition and mood through clinical observation and formal screens. While MC can help with spasticity, the Modified Ashworth Scale (MAS) doesn’t pick up on effects. Therefore, client-specific evaluations should be used.
MC impacts memory, learning, and attention. Keeping this in mind, when practitioners plan interventions, they should take impaired cognitive skills into account and possible schedule treatments outside of acute use.2 The article notes that people who use MC say that they develop a tolerance and claim limited or no impairing side effects. Moreover, people who use MC should avoid driving for four hours after inhalation and six hours after ingestion, so community mobility may be impacted. Lastly, since MC can increase blood pressure and heart rate, vital signs should be monitored during exercise because of an increased risk for acute myocardial infarction.
A blog post from Harvard Medical School says that side effects from CBD include nausea, fatigue, and irritability. It can also increase the efficacy of certain medications “by the exact same mechanism that grapefruit juice does.”12 The Medline Plus website has some helpful information about potential drug interactions as well as recommended dosages for Epidolex.13 The National Center for Complementary and Integrative Health says that more research needs to be done to develop a comprehensive understanding of the health effects of MC and that steps should be taken to overcome regulatory barriers to research.11
What is the Role of OT?
An OT, alongside the health care team or with an individual client, may be able to help address and assess the whole person – mind, body, and spirit, and look at the root cause of symptoms, client factors, or interferences to optimal occupational performance. An OT may be able to assist determining what approaches may be helpful instead of or in addition to cannabis products when all other means have been considered.
For example, if a client is experiencing pain or anxiety an OT can assess, alongside other health professionals, what may be at the root cause of these symptoms and support a client with integrative health approaches that are efficacy-based to lower pain and anxiety, through a comprehensive OT plan of care.
OTs may be able to provide education and help clients improve medication management skills. It is not in OT scope of practice to recommend medications or supplements. If educated, an OT may be able to share with clients and the medical team the risks and benefits of cannabis or support a client with cannabis when and if appropriate within state laws.
Over time, as cannabis laws may change to include accessibility in additional states, more research for potential risks and benefits and the role of OT will likely become more clear. Know your state laws and refer the client back to a physician or referring practitioner for medical evaluation and prescription recommendations.
References
- Marijuana and Cannabinoids. (2018, October 25). Retrieved May 14, 2019, from https://nccih.nih.gov/health/marijuana
- Bell, A. (2018, December 10). An Introduction to Medical Cannabis and Occupational Therapy. Retrieved May 14, 2019, from https://www.aota.org/Publications-News/otp/Archive/2018/medical-cannabis.aspx
- World Health Organization. (2017, November 10). Cannabidiol (CBD): Pre-Review Report [PDF]. Geneva.Expert Committee on Drug Dependence Thirty-ninth Meeting. Retrieved June 16, 2019 from https://www.who.int/medicines/access/controlled-substances/5.2_CBD.pdf
- CBD Project. (n.d.). What is CBD? Retrieved from https://www.projectcbd.org/cbd-101/what-is-cbd
- Holistic Occupational Therapy. (n.d.). In Facebook [Group Page]. Retrieved June 16, 2019 from https://www.facebook.com/groups/holisticoccupationaltherapy/
- Hampson, A. J., Grimaldi, M., Axelrod, J., & Wink, D. (1998). Cannabidiol and (2)D9-tetrahydrocannabinol are neuroprotective antioxidants. Proceedings of the National Academy of Sciences of the United States of America, 95(14): 8268-8273.
- Wolf, S. A., Bick-Sander, A., Fabel, K., Leal-Galicia, P., Tauber, S., Ramirez-Rodriguez, G… & Kempermann, G. (2010). Research Cannabinoid receptor CB1 mediates baseline and activity-induced survival of new neurons in adult hippocampal neurogenesis. Cell Communication and Signaling, 8(12).
- Pacher, P., Bátkai, S., & Kunos, G. (2006). The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacological Reviews, 58(3): 389-462.
- Pacher, P., & Kunos, G. (2013). Modulating the endocannabinoid system in human health and disease: successes and failures. The FEBS Journal, 280(9): 1918-1943. doi: 10.1111/febs.12260
- MacCallum, C. A., & Russo, E. B. (2018). Practical considerations in medical cannabis administration and dosing. European Journal of Internal Medicine, 49, 12–19. doi: 10.1016/j.ejim.2018.01.004
- Marijuana and Cannabinoids. (2018, October 25). Retrieved June 16, 2019, from https://nccih.nih.gov/health/marijuana
- Grinspoon, P., MD. (2018, August 24). Cannabidiol (CBD) – what we know and what we don’t. Retrieved from https://www.health.harvard.edu/blog/cannabidiol-cbd-what-we-know-and-what-we-dont-2018082414476
- Cannabidiol: MedlinePlus Supplements. (2018, October 29). Retrieved June 16, 2019, from https://medlineplus.gov/druginfo/natural/1439.html




Leave a Reply